In today’s competitive and cost-constrained healthcare environment, hospital financial leadership is increasingly asked to justify every capital investment not just on clinical merit, but on financial logic. Hygiene and disinfection are no exception.
This guide distills the key financial metrics like ROI, total cost of ownership (TCO), depreciation, compliance risk, and shows how UV Smart’s D60 stands out as a smart, defensible investment in the pursuit of safer, more efficient care.
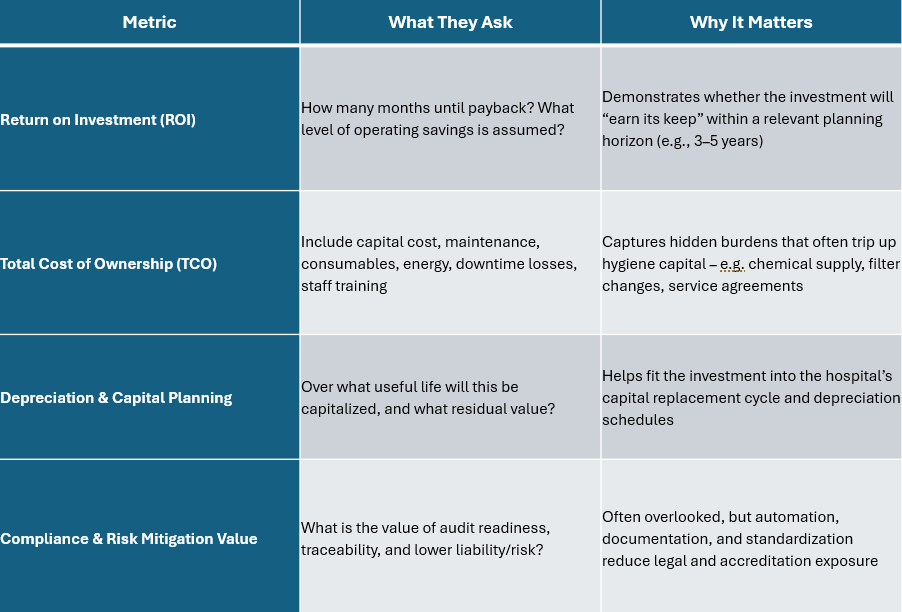
Key Metrics Hospital Financial Leaders Use to Evaluate Hygiene Technology
Before approving a hygiene investment, financial leadership we work with said they focus on clarity in four core metrics:
How Traditional Disinfection Stacks Up (and Where It Breaks Down)
It helps to review the limitations and hidden costs of conventional disinfection methods:
- Consumables & chemical costs: Many systems rely on repeated chemical purchase, dilution control, protective gear, and disposal. Over time these recurring costs accumulate.
- Labor and process variation: Manual wiping or soaking is sensitive to human error, variance in dwell times, and compliance drift.
- Device damage and repair: Harsh chemicals degrade seals, adhesives, optics, and surfaces, driving repair or replacement costs.
- Downtime & throughput constraints: Traditional washer-disinfectors or soak-based cycles can take tens of minutes (or more) including drying and cooling phases. Many scopes or probes lie idle, reducing throughput and squeezing revenue potential.
- Traceability and audit burden: Manual processes often lack auto-logging or robust validation, creating gaps in compliance or audit challenges.
Why the UV Smart D60 Delivers on Financial Logic
Here’s how the D60 aligns with the four critical decision metrics above, backed by internal and external evidence:
ROI / Payback Potential
- The D60 disinfects channel-less ENT scopes or TEE probes in 60 seconds per cycle (plus minimal pre-cleaning) which is dramatically faster than many conventional cycles.
- Because it requires no consumables, no chemical reagents, no water, and very low energy, its operating cost per cycle is exceedingly low.
- The D60 saves time, reduces repair costs, cuts CO₂, enables more throughput. You can see the cost savings for your facility by using our cost calculator.
- In comparative testing, the D60’s disinfection efficacy was found to be as effective as standard Cidex OPA protocols for flexible laryngoscopes, with no significant difference in microbial reduction.
- This equivalence bolsters confidence that you aren’t trading safety for speed; you’re gaining both.
- The absence of recurring consumable and chemical costs means that beyond payback, nearly all further cycles contribute to bottom-line savings. Learn more about the Green Standard and how UV Smart is committed to reducing waste in infection prevention tactics.
TCO & Lifecycle Costs
- No consumables: Because the D60 uses UV-C light rather than chemicals, the ongoing ingredient cost is essentially zero.
- Low energy usage: The D60 contains 8 lamps that fire for only 60 seconds per cycle and automatically shut off if the lid is opened mid-cycle.
- Minimal maintenance & service burden: No tubing, pumps, chemical mixers, filters, fewer mechanical failure points.
- Reduced repair costs for scopes: Because UV-C is non-corrosive and doesn’t degrade materials, it avoids the gradual wear effects that harsh chemicals impose on delicate optics and seals. Reduced repair costs are a key value driver.
- Simplified inventory & logistics: Because cycles are fast, fewer backup scopes may be needed, lowering capital tied up in inventory and the logistical costs of transporting scopes to central sterilization units.
Thus, the lifetime operating cost per cycle is extremely low, making the D60 highly efficient from a cost-per-use standpoint.
Depreciation & Capital Planning Fit
- The D60 is a capital asset and can be depreciated over its useful life in compliance with hospital accounting standards (e.g. straight-line over 7–10 years, depending on local regulation).
- Because the per-cycle cost is so low, the primary budget item is the up-front capital, which fits well into capital planning cycles.
- The D60 is an asset, not an expense, converting what would typically be recurring operating cost (chemicals, labor, scope replacement) into a predictable fixed cost.
In practical terms, hospital financial leadership should model scenarios for 3, 5,and 7-year useful lives, compare depreciation profiles, and stress-test sensitivity vs. chemical cost escalation or scope repair inflation.
Compliance, Audit, and Risk Mitigation
- The D60 includes automated traceability: users scan their badge and equipment before and after each cycle, and all reprocessing data is recorded.
- This audit trail supports infection-control committees, accreditation bodies, and internal or external auditors, reducing compliance risk.
- Automated, consistent UV-C cycles remove human variation and error, one cycle, one standard, strengthening process reliability and reducing liability exposure.
- In the event of infection-related incidents or litigation, documented hygiene logs can be powerful defense evidence.
- Particularly for hospitals subject to regulatory scrutiny (public systems, national health services, EU MDR or medical device regulation overlap), the traceability and validation offered by D60 helps align with risk-management expectations.
Implementation& Adoption: Ensuring Success
Even the best financial case can fail if adoption is poor. Here’s how financial leadership can support a smooth rollout:
- Pilot deployment in a high-volume area (e.g. ENT or TEE) and track KPI metrics (cycles/day, disinfection uptime, scope availability, staff satisfaction).
- Stakeholder engagement: Include infection control, clinical leads, central sterilization, biomed, and nursing in selection and process design.
- Training & change management: Ensure staff comfort with new workflows, safety protocols, and auditing requirements.
- Monitoring & ROI tracking: Post-implementation, track real operating savings, and actual uptime to validate the financial case.
- Scale-up plan: Once validated, roll out to more departments (e.g. other endoscopes, ultrasound, flexible scopes) to maximize network effects.
Review our guidance on hospital implementation of UV-C disinfection, including cost and operational implications.
Final Thoughts: Why UV Smart is the Financially Intelligent Choice
Hospital financial leadership views every investment through the lens of risk, return, and accountability. The UV Smart D60 offers:
- Alignment with clinical safety along with financial discipline. Fast cycles, low running cost, minimal consumables.
- It enables traceability and audit readiness, reducing compliance and liability risk.
- It converts recurring chemical + labor expense into a predictable capital cost, with upside in scope protection and throughput.
- Its efficacy is clinically validated (e.g. equivalent performance vs. standard OPA protocols).
By treating hygiene as a strategic investment (not just a necessary cost), hospital financial leadership can drive better safety, more efficient throughput, and demonstrable return like our partner did here. UV Smart is not merely an option, it is a choice grounded in financial logic and rigorous performance.
If you want to experience the impact at your facility, click here to schedule your free trial.








.jpg)
