In women’s health clinics across Europe, two realities exist side by side.
First, HPV is extremely common throughout the European population.
Second, transvaginal ultrasound probes are reused repeatedly every day in busy OBGYN settings.
On their own, neither fact is surprising. Together, they create a clinical environment where disinfection consistency is not just important, but foundational to risk management.
This conversation is not about fear or blame. It is about understanding how prevalence, repetition, and process variability intersect in modern women’s health care.
HPV in Europe Is Widespread
According to the European Medicines Agency, more than 80% of people in Europe will be infected with HPV at some point in their lives, regardless of gender.
The European Centre for Disease Prevention and Control (ECDC) confirms that HPV is the primary cause of cervical cancer, which remains one of the most common cancers among women aged 15–44 in the European Union, with approximately 33,000 new cases and 15,000 deaths each year.
Prevalence data across Europe shows meaningful regional variation:
- Around 9% prevalence of high-risk HPV in Western Europe
- Approximately 17% in Southern Europe
- Up to 21% in parts of Eastern Europe
For women’s health clinics, these figures matter because:
- Many HPV infections are asymptomatic
- Patients are often unaware they carry the virus
- High patient throughput increases cumulative exposure potential
HPV prevalence is not an exception in Europe. It is part of the baseline clinical landscape.
Transvaginal Ultrasound Probes Are Semi-Critical Devices by Design
Transvaginal ultrasound probes come into direct contact with mucous membranes, placing them firmly in the semi-critical category under the Spaulding classification.
This classification exists because mucosal contact carries a higher risk of infection transmission, particularly when devices are reused multiple times per day, as is typical in OBGYN clinics, fertility centers, and women’s imaging departments.
In high-volume European clinics, probe turnaround time is often compressed by:
- Full appointment schedules
- Staffing shortages
- Pressure to reduce patient waiting times
Each reuse cycle increases reliance on process accuracy and consistency.
The Risk Is Not Intent, It’s Variability
Manual probe disinfection workflows depend on multiple human factors:
- Correct product selection
- Proper contact time
- Complete surface coverage
- Ongoing training and adherence
- Accurate documentation
While guidelines exist, manual processes are inherently variable, especially in fast-paced clinical environments.
As UV Smart has explored in its analysis of hospital disinfection workflows, manual reprocessing introduces inconsistency that is difficult to measure, audit, or fully eliminate.
When HPV prevalence is high and often undetected, even small deviations in process reliability become more meaningful.
Why HPV Changes the Risk Equation in Women’s Health
HPV includes non-enveloped viruses, which are generally more resilient to environmental stressors than enveloped viruses. While clinical guidance avoids pathogen-specific guarantees, public health literature consistently highlights that non-enveloped viruses demand robust, validated disinfection processes.
In women’s health settings where:
- Patient volumes are high
- Probe reuse is frequent
- Time pressure is constant
Risk management shifts from individual compliance to system reliability.
This is why infection prevention leaders increasingly prioritize validated, repeatable processes over manual, variable workflows.
When “Routine” Exams Become Repetitive, Risk Accumulates
Transvaginal ultrasound is often described as routine. But routine does not mean low consequence.
Repetition compounds exposure:
- More patients per day
- More probe cycles per shift
- More dependence on flawless execution
In women’s health, where care is intimate and patient trust is essential, the tolerance for variability is understandably lower.
As UV Smart has outlined in its long-term perspective on disinfection strategy, consistency is not about intensity, but about delivering the same validated outcome every time.
Why European Clinics Are Re-Evaluating Disinfection Workflows
Across Europe, women’s health clinics are reassessing probe disinfection as part of broader goals:
- Reducing human variability
- Improving audit readiness
- Supporting staff under operational pressure
- Protecting patient confidence in intimate care environments
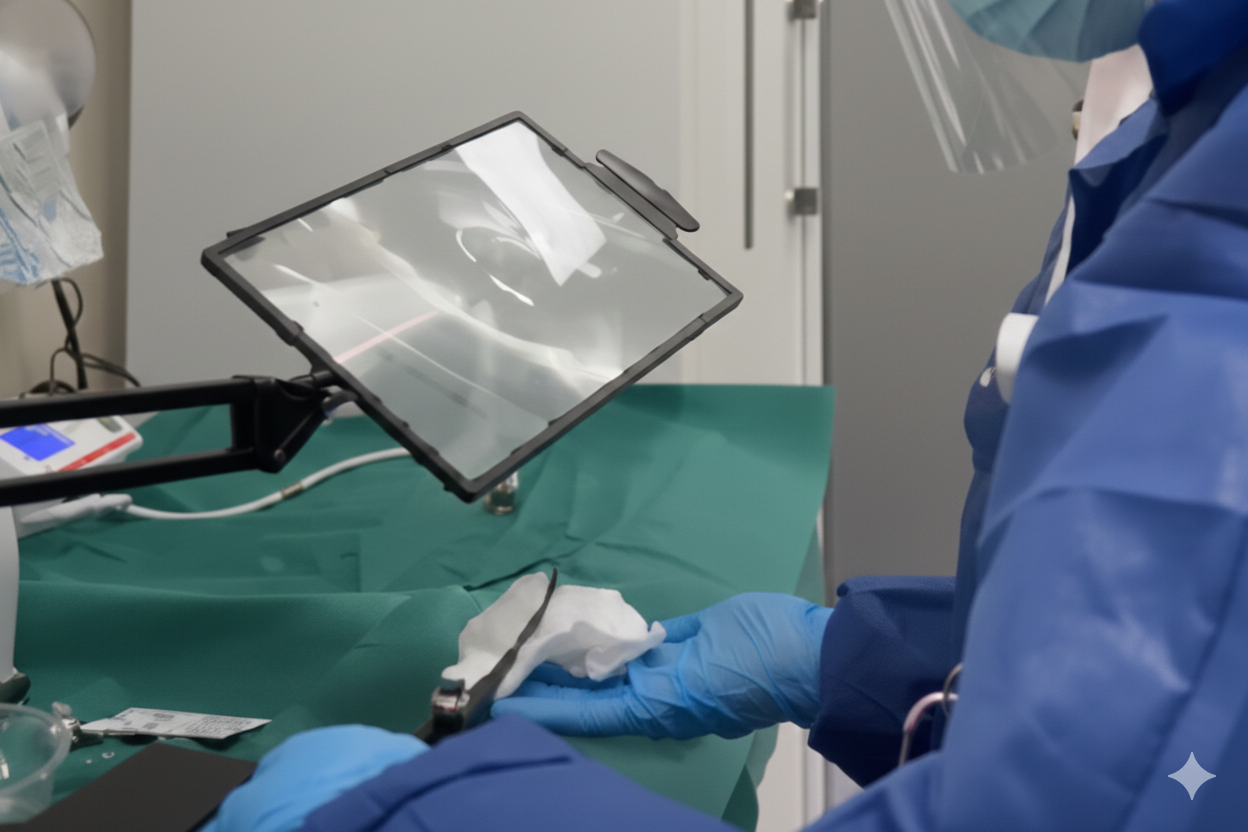
Automated UV-C disinfection is not positioned as a response to one virus, but as a risk-reduction strategy in environments where prevalence and repetition are unavoidable.
UV Smart’s validated UV-C products are designed to provide consistent, documented disinfection outcomes without adding complexity to daily clinical workflows.
Risk Management, Not Alarmism
HPV’s prevalence in Europe does not imply inevitable transmission.
Probe reuse does not imply inadequate care.
But together, they highlight a reality women’s health leaders cannot ignore:
When exposure is common and processes are repeated, consistency becomes the most reliable form of protection.
That is the lens through which disinfection decisions deserve to be made.
Protect Your Patients With UV Smart
Want to see what a real hospital leader thinks? Click here to see a comment left on our LinkedIn page. Then call us learn how validated UV-C disinfection supports consistent, audit-ready workflows for semi-critical ultrasound probes in women’s health clinics, click here to see what a real client think.







.jpg)
