A practical guide for clinicians navigating hospital decision-making
After our most recent blog stirred up lots of responses.
We had several clinicians reached out with similar reactions:
“This makes sense, but we’re not a sales team. Our leadership needs us to explain the value to them. What do we do?”
It’s a great point. Leadership is busy, they get contacted by sales all time. Why is UV Smart different?
We heard your pain.
We're here to help clinicians communicate the organizational impact of UV Smart's products. Clinicians see the friction every day, delayed scopes, manual reprocessing, documentation burden, staff stress, chemical exposure, the list goes on and on. The difficulty is translating those realities into something that resonates with finance, operations, infection prevention, and biomed. We believe a product should positively impact every department. This requires empathizing with your colleagues as you all drive towards the same result.
Below is a practical approach we’ve seen work repeatedly when clinicians want to introduce UV-C disinfection with the UV Smart D60 into budget discussions without turning the conversation into a product pitch.
The key shift is this:
UV-C should be framed as a workforce, flow, and risk-reduction strategy, not just an infection-control purchase.
Start with the staffing reality
Leadership already knows staffing is fragile. What they often don’t see is how much clinical time is consumed by avoidable manual work.
Start with facts they recognize:
· Local vacancy rates
· Overtime trends
· Sick leave and stress-related absence
· Reliance on temporary or agency staff
Much of this data already exists internally. If it’s difficult to access or translate, UV Smart can support clinicians inbuilding a customized business case.
Then connect the dots:
Workforce shortages and burnout are no longer temporary. Without structural changes to workflows, pressure simply shifts onto fewer people, increasing turnover risk and operational instability.
This reframes UV-C from “new equipment” to “how do we protect the staff we still have?”
Show where high-value staff are doing low-value manual work
Next, make the invisible visible.
Map your current disinfection workflow for semi-critical devices such as:
· Ultrasound probes
· ENT scopes
· TEE probes
Highlight where time is lost:
· Transporting devices to central reprocessing
· Waiting for availability or queueing for cycles
· Manual chemical handling and wiping
· Logging, documentation, and compliance steps
Individually these steps seem small. Collectively, they consume hours of skilled clinical time per week, slow patient throughput, and create bottlenecks, especially during peak hours.
This is where the conversation starts to shift from infection prevention to patient flow.
Quantify the impact using ROI calculators
Once the workflow is clear, numbers do the work for you.
Using the UV Smart D45/D60 Cost & ROI Calculators you can model your own department and show:
· Hours freed per year
· Full-Time Employee-equivalent capacity regained
· Reduction in overtime pressure
· Hard savings on chemicals, wipes, water, and maintenance
· Estimated payback period
Finance teams respond to time-bound ROI and realistic assumptions. These calculators are built specifically to support internal discussions, not marketing claims.
For many hospitals, this is where UV-C shifts from “nice idea” to “why are we still doing this manually?”
Expand the business case beyond staffing
Staffing is often the entry point, but it shouldn’t be the only argument.
Better patient flow
· Faster turnaround of probes and scopes
· Fewer delays or rescheduled exams
· Less waiting between patients
Improved availability directly supports throughput, utilization, and patient satisfaction metrics leadership already tracks.
Less device damage and rework
Non-UV-C reprocessing methods increase risk of:
· Probe surface degradation
· Connector damage
· Premature repairs or replacements
Automated UV-C eliminates repeated chemical exposure and excessive handling, helping extend device lifespan and reduce unplanned costs.
Lower operational risk
Manual processes introduce variability:
· Different techniques
· Different dwell times
· Documentation gaps
Validated, automated UV-C helps standardize outcomes, reducing audit risk and compliance exposure.
5. Tailor the message to each decision-maker
Doctors don’t need one proof point, they need the right proof point for the right audience.
What to say to Infection Prevention (IPC)
· Consistent, validated high-level disinfection
· Reduced human variability versus manual processes
· Stronger audit readiness and traceability
· Support for MDR compliance and policy alignment
Message: This improves reliability and reduces risk, not shortcuts safety.
What to say to Finance
· Measurable ROI using your own volumes
· Reduced overtime and hidden labor costs
· Lower spend on chemicals, wipes, water, and repairs
· Predictable payback period
Message: This is an operational efficiency investment with defensible numbers.
What to say to Operations / Nursing Leadership
· Faster turnaround times
· Fewer workflow bottlenecks
· Less task switching and rushing
· More predictable shifts
Message: This stabilizes daily operations and reduces burnout.
What to say to Biomedical / Clinical Engineering
· Less chemical exposure to sensitive devices
· Fewer repairs related to handling or degradation
· Simplified maintenance planning
· Clear validation and documentation
Message: This protects assets and reduces downstream workload.
What to say to Sustainability / ESG teams
· Thousands of kWh saved annually
· Thousands of litres of water eliminated
· Over 8,600kg of CO₂ avoided per year
Message: This supports hospital sustainability goals without compromising care.
Make it human
Finally, bring it back to the people.
By removing repetitive, manual disinfection tasks and long turnaround times, you’re not just improving efficiency, you’re giving clinicians:
· More time with patients
· Fewer end-of-shift backlogs
· More predictable workdays
· A tangible reduction in daily friction
In a strained workforce environment, that matters.
The takeaway
When UV-C is framed only as an infection-control line item, it competes with dozens of other priorities.
When it is framed as a workforce, flow, and risk-reduction strategy, supported by real data and tailored to each decision-maker, it becomes much harder to dismiss.
Clinicians don’t need to be salespeople to start that conversation.
They just need the right proof points.
If you want help running your own numbers or preparing for internal discussions using the D60, UV Smart is happy to support you.
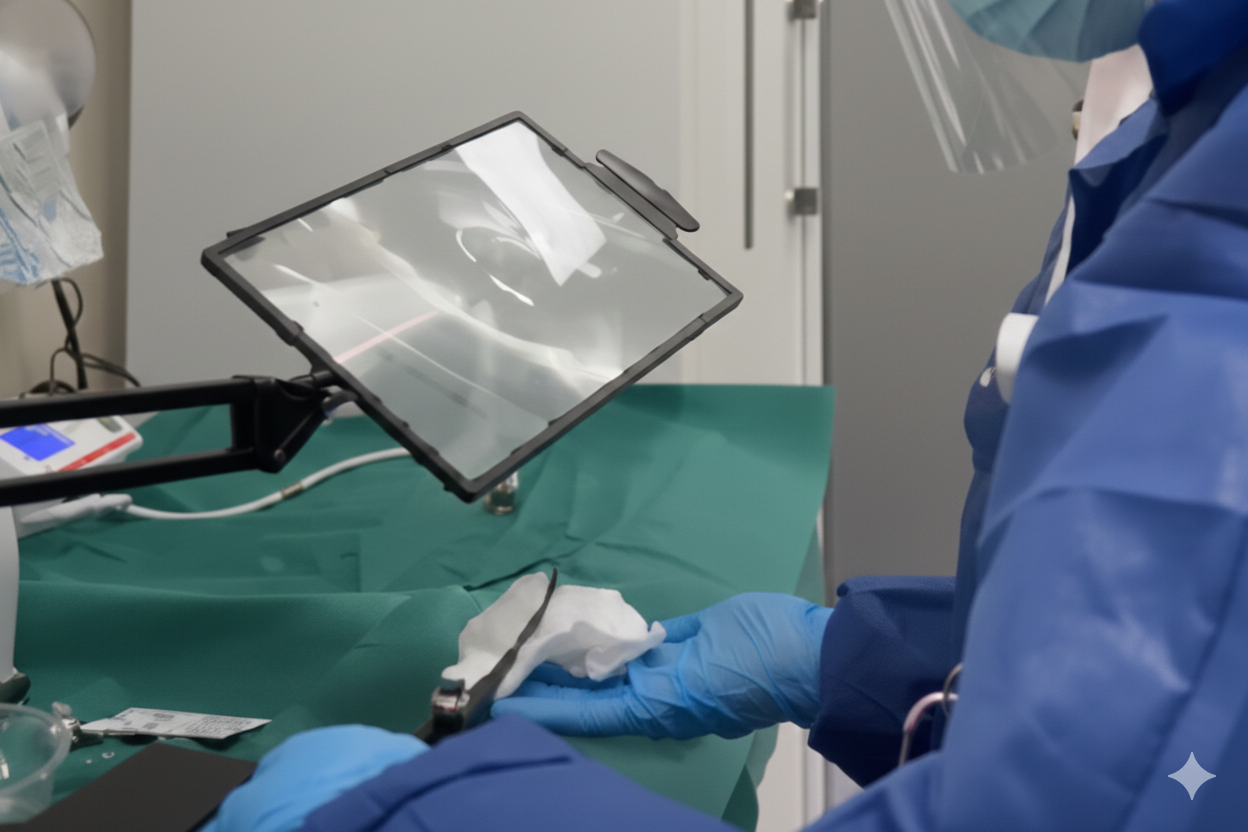
Or see the D60 or D45 in action for yourself, for FREE.




.jpeg)


.jpg)
