Ultrasound Probe Disinfection with Wipes: Not as Disinfected as You Think
Wipes and foams are commonly used for disinfecting ultrasound probes, TEE probes, or ENT scopes. On the surface, they appear convenient: quick application, chemical action, and low upfront cost. But under that surface lies a host of unspoken risks and inconsistencies.
A User-Dependent Process
Manual disinfection with wipes depends entirely on the user. Application contact time, wiping technique, drying, and even coverage can vary from person to person, shift to shift. No machine oversees the process. No sensors confirm if the chemical actually made contact for the required time. No audit trail exists.
Clinical Guidelines vs. Real-World Risk
Clinical guidelines may accept manual high-level disinfection, but the reality is more complex. Ultrasound probes used in semi-critical procedures, such as transvaginal or transrectal scans, must be reliably disinfected. If not, patients risk exposure to HPV, bacteria, or viral pathogens.
Evidence from Studies
Multiple peer-reviewed studies and clinical evaluations have raised concerns over wipe efficacy on ultrasound probes. In many cases, wipes are used on devices that are hard to wipe completely, particularly around seals or irregular probe heads. These limitations make “complete disinfection” more of a hope than a guarantee. Contact us to learn more about these publications.
Risk of Equipment Damage
There’s also the issue of cumulative damage. Some chemical agents can affect probe materials over time, especially if not wiped or dried properly. Reprocessing practices that depend on human consistency open the door to safety gaps.
Wipes may be the current standard in many hospitals, but “standard” should never mean “good enough.”
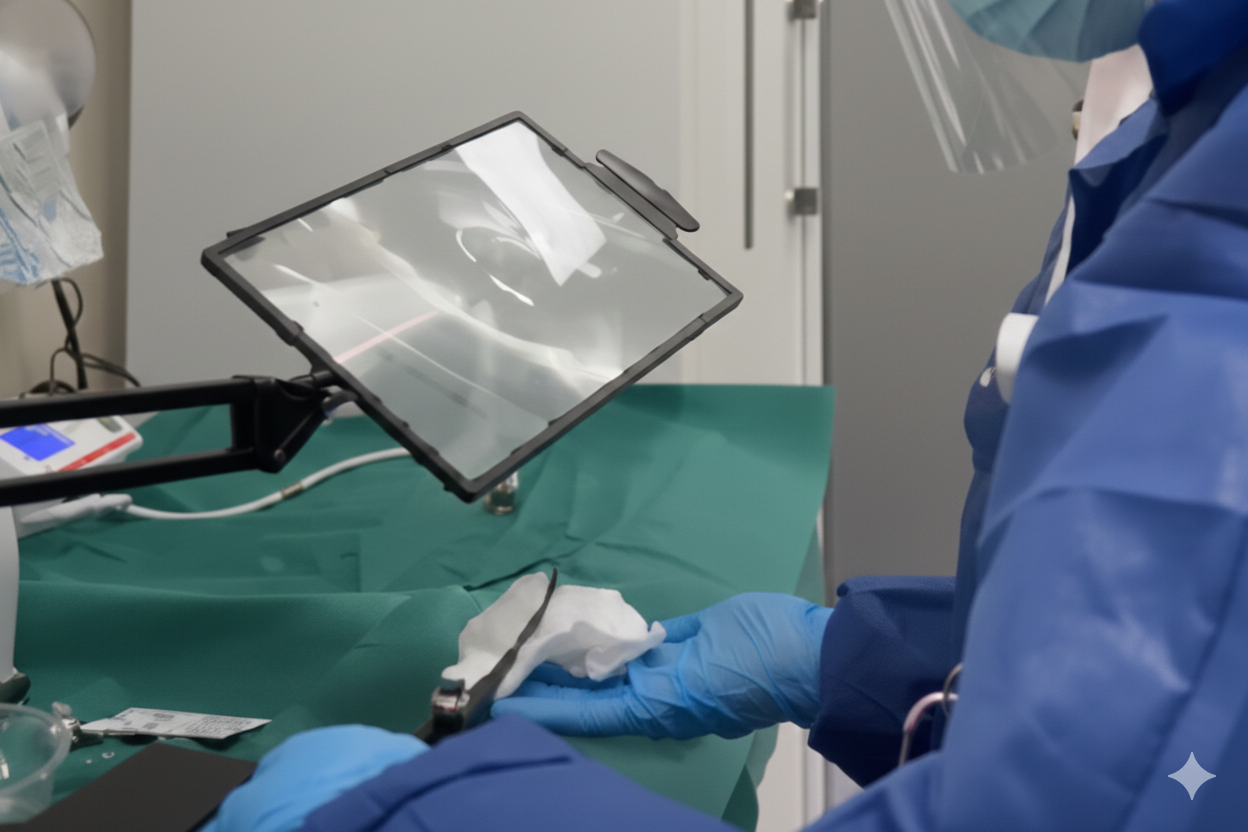
Manual Disinfection for ENT Scopes and TEE Probes: A Dangerous Illusion
For ENT scopes and TEE probes, manual disinfection is often treated as a shortcut, an improvised solution in settings where automated methods are too unavailable, too costly or too slow. But this shortcut introduces serious clinical risks.
Why Wiping is Flawed
Manual wiping of ENT endoscopes or TEE probes is not only difficult, it’s fundamentally flawed. The narrow tips, fiber optics, and textured materials of ENT endoscopes and TEE probes make them hard to disinfect manually. It’s easy to miss hidden surfaces. It’s hard to apply consistent pressure. And unlike with rigid devices, it’s nearly impossible to confirm full coverage.
False Security from Quick Fixes
Yet hospitals still use soaking trays or wipes as quick fixes, unaware of the potential consequences. High-level disinfection means reducing bacterial load. In reality, most manual methods rarely approach this. Even when done meticulously, the outcomes remain unverified.
Lack of Proof and Documentation
There’s no data logging, no quality control, no documentation. If an infection is traced back to an ENT scope or TEE probe, proving disinfection was done correctly is nearly impossible.
The Need for Validated Alternatives
Instruments like TEE probes and ENT endoscopes are semi-critical devices. They contact mucous membranes and can transmit pathogens. As such, they deserve a validated, reliable, and traceable disinfection process and not a rushed wipe-down.
With UV-C systems entering the market that meet guideline requirements, it’s time to retire the illusion that manual equals disinfected. Hospitals should no longer accept the liability of invisible failures.
Discover an automated, faster, and fully traceable alternative to manual wiping, contact us today or explore our products!







.jpg)
