In healthcare, performance is often measured in speed. But in clinical care, speed without control introduces risk, especially when it comes to high-level disinfection (HLD). Hospital leadership must therefore balance operational efficiency with patient safety, audit readiness, and reproducible outcomes.
High-level disinfection workflows are evaluated not by how fast they run, but by how reliably they prevent pathogen transmission through validated methods. This framing aligns with international infection prevention frameworks, including the Spaulding Classification and organizations such as the CDC (which specify the appropriate level of disinfection based on device classification) and emphasize the importance of validated processes.
Clinical Turnover Pressure Is a Leadership Challenge
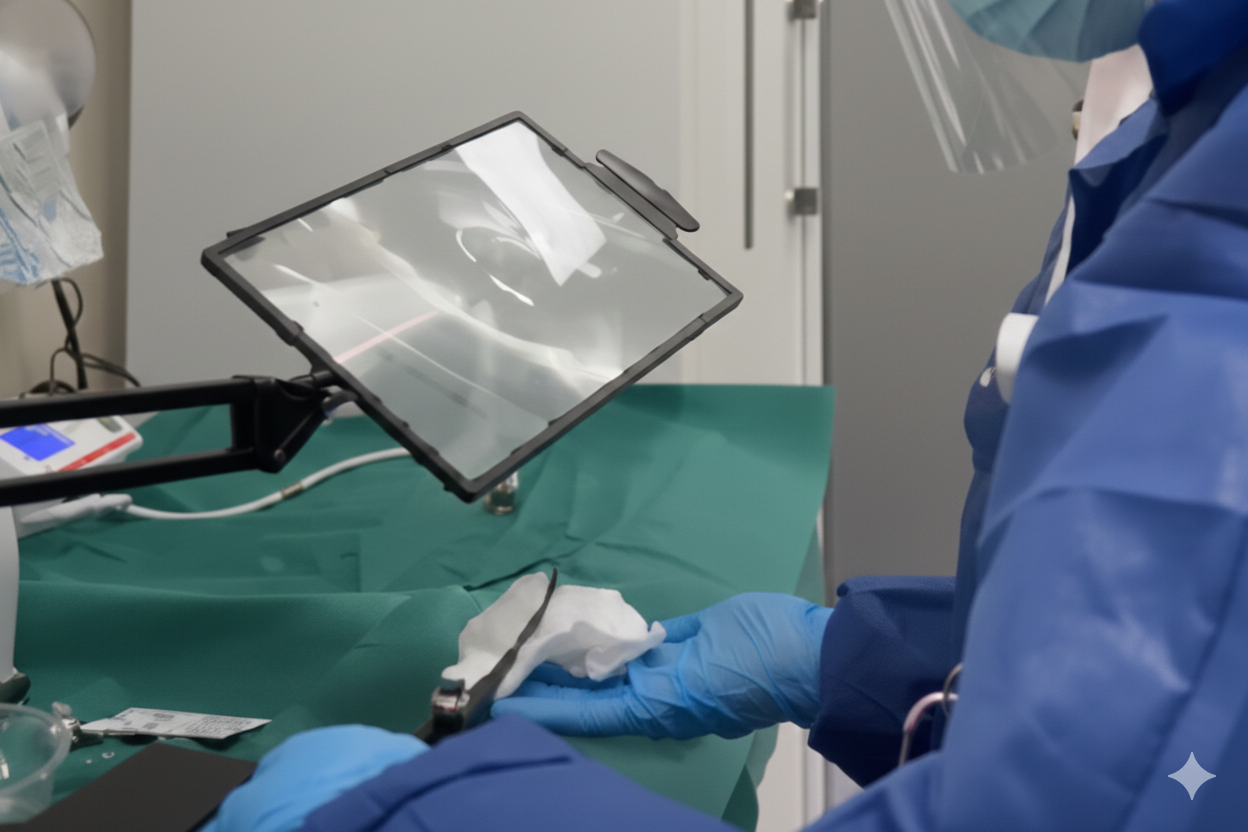
Departments, such as cardiology departments, rely on transesophageal echocardiography (TEE) probes and other semi-critical devices for diagnostic and interventional workflows. These probes require high-level disinfection between uses, aligning with guidelines that specify chemical HLD with validated processes for semi-critical devices.
Leadership in hospitals must also ensure that reprocessing aligns with regulatory frameworks and best practices across regions such as:
- CDC healthcare disinfection guidelines (US)
- European standards for medical device reprocessing and UV-C inclusion
- National frameworks like NEN 8281:2025 that explicitly validate UV-C as a safe, effective disinfection method in hospital workflows
These frameworks emphasize validated and controlled processes, consistent documentation, staff safety, and process reliability, not speed in isolation.
The Hidden Risk of “Faster” Disinfection
Traditional HLD workflows often introduce variability when time pressure increases. Manual steps can create inconsistencies; long soaking times delay probe availability; chemical handling can expose staff to occupational risk; and rinsing/drying adds another layer of complexity.
Real consistency, the kind that auditors and infection prevention teams require, comes from systematic, validated processes, not rushed manual execution. Chemical HLD also requires multiple handling steps that can introduce risk points, including rinse and drying stages that are prone to contamination if not managed perfectly.
UV-C Changes the Risk Equation
Ultraviolet-C (UV-C) disinfection value stems from controlled, validated implementation, where exposure doses, consistent cycle conditions, and repeatable workflows support high-level disinfection outcomes on semi-critical devices. Hospitals that embrace UV-C for HLD do so because:
- The technology has been validated in clinical settings
- Systems are engineered for consistent disinfection cycles
- Traceability and audit documentation are built into workflows
UV-C systems that are medically certified and designed for healthcare use align with regulatory expectations and evidence frameworks for validated disinfection with fewer steps, no chemical handling, and reduced risk of residual contamination.
Evidence for UV-C Efficacy with TEE Probes
TEE probes, critical tools in cardiology, require high-level disinfection after every use. According to CDC framework and semi-critical device reprocessing guidelines, TEE probes should be cleaned and disinfected with high-level methods after each use.
Independent studies show that UV-C HLD can achieve potent sporicidal effects and validated disinfection outcomes for TEE probes. For instance:
- UV-C exposure has been found to produce strong sporicidal activity in comparison to chemical HLD methods within short exposure times.
- UV Smart’s D60 system, designed for TEE probes and other semi-critical devices, is registered as a Class IIa medical device and has been clinically evaluated to reduce colony-forming units on TEE probes in hospital settings.
These results support the conclusion that UV-C, when properly engineered and validated, delivers high-level disinfection performance comparable to traditional methods while supporting the workflow needs of high-throughput cardiology departments.
Alignment With European and US Guidance
Across regions, infection prevention authorities emphasize:
- Validated disinfection methods that can be documented and audited
- Traceability of reprocessing cycles
- Worker safety and reduced chemical exposure
- Consistent outcomes regardless of staff turnover
National initiatives such as the Dutch NEN 8281:2025 and Swiss GPAE standard formally recognize UV-C as safe and effective for non-critical and semi-critical disinfection, giving hospitals clear regulatory support for implementing UV-C systems in real workflows.
This represents an evolution in how national standard bodies and regulators validate not just method, but application and workflow integration, a key benefit for hospital decision-makers.
Faster Turnover - Safely
From a leadership perspective, the safest technologies are those that:
- Minimize manual variability
- Support audit-ready documentation
- Reduce occupational exposure
- Align with regional infection prevention standards
- Demonstrate consistent performance across repeated cycles
In practice, this means speed is a consequence of good design, not the primary objective. When UV-C HLD is engineered and validated correctly, faster turnover becomes synonymous with safer, more predictable clinical workflows.
The Takeaway for Hospital Leadership
High-level disinfection should be evaluated on the safety and organizational impact. UV Smart designs its products to address a comprehensive risk management system that protects patients, preserves device integrity, and supports consistent, reproducible outcomes.
For cardiology departments using TEE probes and other semi-critical devices:
- UV-C HLD systems provide documented performance
- Regulatory and standards bodies increasingly endorse UV-C when validated for healthcare use
- Workflow efficiency and safety can co-exist in fast-paced clinical settings
UV-C high-level disinfection helps hospital leaders achieve both throughput and safety without sacrificing audit readiness or clinical confidence.
Connect With Us
Want to see the D60 in action for yourself? Start your free trial, watch how it seamlessly integrates into your organization, and the positive impact it has on your workflow.







.jpg)
